City Council has light night
My Colonoscopy and Me, SHINE-ola is next week, Death toll drops plus headlines
Note to subscribers: An annual or monthly subscription is billed to your debit or credit card as ARKANSAS.SUBSTACK.COM and if you have questions, please email arkansas@substack.com. Thanks for reading and subscribing!Death toll drops
The weekly death toll from the ongoing pandemic dropped as the total number of dead Arkansans was at 16, but that number might be might lower due to a lag in reporting from the July 4 holiday on Monday.
The previous week it was at 28 and the week before that it was 24.
The total number of dead Arkansans is now at 11,596.
As for the national trends, the forecast numbers from the Centers for Disease Control are below and through July 30.
The forecasts are all over the place in both weekly death counts and total deaths. The top left hand chart is new weekly deaths forecast and that ranges from over 100 to single digits on the low end. The number of total deaths is close to or exceeding 12,000.
If you don’t want to get sick and die, there’s some things you can do:
Get vaccinated
Get boosted
Wear a mask
Avoid crowdsThe Headlines
Wildwood seeks adult performers for Oliver, Spamalot: The Wildwood Park for the Arts is putting on Oliver this fall and they’re looking for actors. Adult actors this time and not just for Oliver, as they’re also seeking adult actors for a production of Spamalot
Auditions will be Monday, July 18 and will start at 5 p.m.They’ll be held at the Cabe Theater at Wildwood Park for the Arts.
Auditions are by appointment and to schedule email, Zachary Rhodes at at zach@wildwoodpark.org who will also provide instructions on what’s needed. To read more, click here.
Seniors with prediabetes should eat better, get moving, but not fret too much about diabetes
Upcoming meetings: The North Little Rock School Board will meet tonight. The North Little Rock City Council will meet Monday night and the North Little Rock Planning Commission will meet Tuesday afternoon.
SHINE-ola to be July 14: The Inaugural SHINE-ola will be held on Thursday, July 14 at South on Main. The show will start at 6 p.m. and is scheduled to run for four hours. The address for South on Main is 1304 Main St., in Little Rock. Tickets are $7 and can be purchased by calling 501-244-9660 or at the door the day of the show.
Covid toolkit
There’s now a one-stop shop to learn about vaccination sites and other Covid related information. Click here to learn more.
Travs at home
The Arkansas Travelers complete their series against Springfield this week with fireworks on Friday night and the always popular Kids Day Bash on Sunday afternoon.
Homestand
Today... 6:35 p.m. … vs. Springfield; Promotions: $3 Thirsty Thursday and Noche De Diamantes
Friday ... July 8 ... 7:05 p.m. … vs. Springfield; Promotions: Fireworks
Saturday ... July 9 ... 7:05 p.m. … vs. Springfield; Promotions: T-Shirt Giveaway and Kids Run The Bases
Sunday ... July 10 … 1:35 p.m. … vs. Springfield; Promotions: Kids Day Bash and Team Card Set Giveaway
Road swing
Tuesday ... July 12 ... 7:05 p.m. ... at Wichita
Wednesday ... July 13 … 12:05 p.m. ... at Wichita
Thursday ... July 14 ... 7:05 p.m. ... at Wichita
Friday ... July 15 ... 7:05 p.m. ... at Wichita
Saturday ... July 16 ... 6:05 p.m. ... at Wichita
Sunday ... July 17 … 1:05 p.m. ... at Wichita
Maumelle: City Council report
Tuesday night’s meeting was brief with only one agenda item, so I’ll be brief as well.
Doreen Mattes, our city’s HR Director gave a brief update on things going on in Maumelle. As I’ve previously written about, our city will be transitioning to an online human resources system in the coming months, this will offer substantial time savings for our department heads and supervisors as they process payroll every two weeks. Maumelle’s current employee count is 264 employees which includes 178 full-time employees and 86 part-time employees. During the summer months, our number of employees grows with so many part-time workers in the Parks and Rec department.
The only agenda item of the week was a budget resolution for Maumelle Animal Services.
This budget adjustment doesn’t affect the city’s bottom line, but simply reflects actual income and expenses in Animal Services. For the year, we’re budgeting $10,500 in adoption fees (revenue) and an expense of $10,500 for veterinary services. Additionally, residents have made donations directly to Maumelle Animal Services this year in the amount of $1,538. At the request of Chris Davis, Animal Services Supervisor, the council appropriated those funds to be used for animal medical expenses.
Since we’re talking animals, let me encourage you to drop by and support our animal shelter with your time.
One of the best things you can do is spend time playing with the dogs and cats that are in our shelter. This helps the animals adjust to people, plus it’s fun! My family has been going to the shelter once or twice a week to play with the animals and it’s a good summer activity. If you’ve got kids, grandkids, or you’re a kid at heart, a few minutes a week at the shelter will help these animals tremendously.
That’s all for the week, if you have any questions or concerns, please let me know. Chad. 501-529-1336, chad4maumelle@gmail.com
My Colonoscopy and Me
At a certain age, you’re supposed to get a colonoscopy.
For me, that certain age came and went a couple of years ago, but in my procrastinating defense, it didn’t seem wise to take up valuable healthcare resources for a purely preventive issue during the early days of a pandemic.
For me, I had lots of questions that didn’t seem to have any good answers, so what follows is a personal journey through the process of going from wanting a colonoscopy to a few days after having the exam.
Navigating healthcare isn’t easy. It is complicated by design and prone to frustration, but having a trusted provider will help tremendously. In my case, I didn’t.
Step 1 - So, you want a colonoscopy
A colonoscopy is, for those with insurance, a covered preventive procedure, akin to having your teeth cleaned. Any cost associated with the exam is minimal compared to what it costs to treat the gut cancers.
So, with that in mind, now is the time to navigate your insurance provider’s coverage portal to determine what clinic is covered. Your employer’s human resources office can also be extremely helpful in this situation, or you can ask your doctor, or their nurse, at an exam. Again, if you have hit 50, and don’t have any family health history, you’re the right age for one, and it is very likely your doctor will suggest it then.
Step 2 - The initial visit
My insurance provider said GastroArkansas was the clinic for me. I scheduled my initial appointment online, and they followed up with a call to confirm.
The office visit itself was very basic. They take your blood pressure and run through your medical history. The colonoscopy generally follows in a few days. In my case, due to a medical allergy, that was a couple of weeks later.
They also do their best to answer your questions. Here’s some important ones to ask:
What time will the appointment be?
What are the dietary restrictions on the day before and day of?
Will the day-before prep medication be over-the-counter or prescription?
What are the most likely complications or issues that could happen before or after the procedure?
As to the first question, if you have a choice on time, pick as early as possible. Like most other procedures, you won’t be able to have anything to eat or drink after midnight preceding the colonoscopy.
As to the second, you’ll be on a soft foods/liquid diet the day before. You can also have hard candy. There are some limitations on what color Jell-O you can have, so no red, no purple. That’s also true for the Gatorade that some prep regimens will have you drink the day before.
The over-the-counter vs. prescription prep is really, really important and will vary by provider as well as your family medical history.
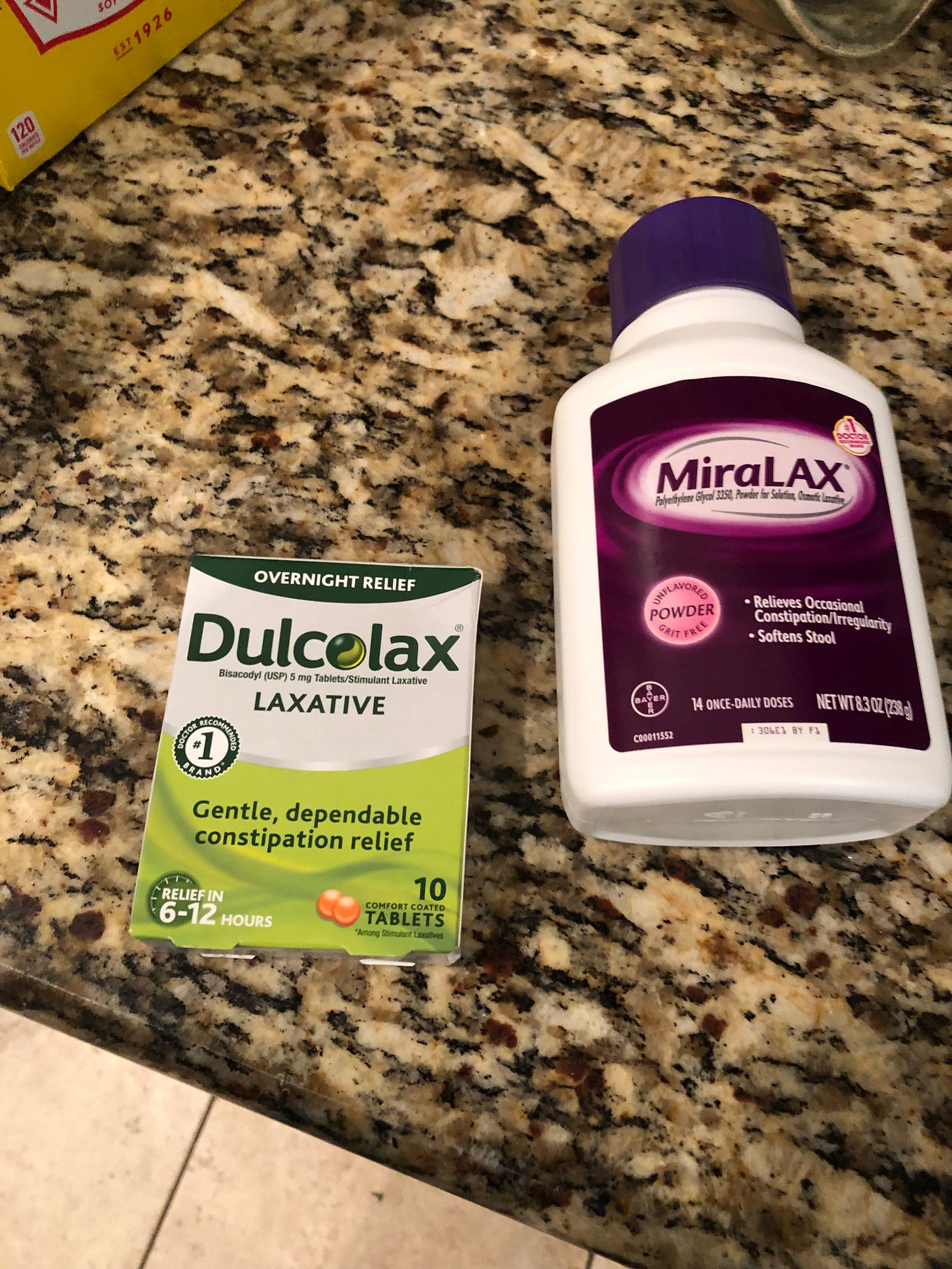
In my case, my prep was OTC and all things that could be purchased at Kroger, specifically, a 238 gram bottle of Miralax, a laxative powder that is mixed with Gatorade, and Dulcolax, a laxative pill.
Both are in the pharmacy section at Kroger. You can also purchase both at Walgreens or Walmart or your local pharmacy.
I bought a big bag of Jolly Ranchers, Gatorade, ginger ale, and orange Jell-O, and from the pantry got bouillon cubes. Also, coffee. Black coffee.
Step 3 - Prep day
Prep is pretty awful and the worst part of getting a colonoscopy. Because I thought it would be funny, I had also scheduled a dental appointment the morning of prep with the hope the colonoscopy would be that afternoon, but the actual procedure was the next day. It worked out though, in a weird way, because getting a filling replaced meant my mouth and jaw were pretty sore, and I wasn’t much interested in eating the morning of the prep. Not that I could have any real food to eat anyway.
Part 1 of prep was taking four Dulcolax pills at noon. That’s when I discovered I had mistakenly purchased suppositories instead of tablets, which meant an extremely quick trip to Walgreens, so the pills were taken at 12:15 p.m. instead.
(Also, for sale: four suppositories, never used.)
Things were fine, and being blessed with a work-from-home job meant I had easy access to a bathroom. That’s important!
If you have an office job or work really anywhere, I’d highly encourage you to take half a sick day for prep and go home at lunch and not come back that day or the next day.
Pro tip: If you feel like you need to go to the bathroom, go to the bathroom. Don’t hesitate. Just go.
For the purposes of reporting, I logged my first bathroom trip at 1:30 p.m. last Thursday. What followed was a hazy blur of bathroom visits that continued through the afternoon and into the night. They were only broken up by 32 ounces of Gatorade mixed with half a bottle of the Miralax at 4 p.m., followed by the same cocktail at 8 p.m.
The Miralax mixes up smoothly with the Gatorade, unlike, say, Metamucil.
I gave up on logging the individual times, but from the first visit to the last trip before bed, I made a total of 15 bathroom visits in roughly nine hours.
Again, it was awful. But a small bowl of ice cream before going to bed made the day better.
Step 4 - The day of
Friday morning came early for a 7 a.m. check-in at St. Vincent’s in Little Rock. I made another trip to the bathroom, none during the night though, then had a shower and got dressed. You can’t
have anything to eat or drink at this point, and you’ll need someone to drive you to the clinic or hospital as you won’t be able to drive home since you’re sedated during the procedure.
For the curious, I weighed the morning of prep and the morning of, and I dropped not quite six pounds of, umm, waste.
Dropped at the door, I checked in, then did more paperwork that morning and got wristbanded up along with a sticker to wear. You can pretty much wear whatever you want the day of because you’ll change into a gown for the actual exam.
You’ll check in at the GI lab next, and then do more paperwork – take a pen – and wait some more to be called back. My appointment was at 9 a.m., and that’s roughly when I was called back to put my things in a bag and change into a gown.
Then the future comes and hits you in the face as you get on a gurney, with nothing but a snapped-together gown on, and you begin getting hooked up to various things: EKG stickers along your chest for the heart monitor, then an IV stick for a blood draw in your hand. When that’s not successful, you get an IV stick in your other hand for a blood draw and a bag of fluids. Then you wait some more.
Then the anesthesiologist makes an appearance, runs through some questions, and then you get wheeled across the hall to an exam room. There the anesthetist riddles you with more questions, and in my case, genuine curiosity about my medical allergy. Then the gastroenterologist comes in, says hello, makes small talk about the prep, and asks you to roll on to your side. The anesthetist says he’s about to push the drugs and that you might feel a slight burn. I quickly checked my watch, and that’s it. What happened next I do not have any notion of because I was sedated and unconscious.
A short 15 minutes later, I woke up with a start, similar to the one you get when you fall asleep at the airport and don’t understand where you are or why it is so noisy, then you remember where you are. The nurse brought me a Diet Shasta to drink from a straw while waiting the 30 minutes to make sure I had no ill effects from being sedated.
At some point, the doctor called my wife to give her a report that “he has the colon of a 20-year-old” and there were no polyps and nothing to biopsy. Then the doctor came and told me the same thing as well and I wouldn’t need to come back for a decade.
I didn’t feel sore. I didn’t really feel anything besides being very hungry. I waited for my wife to pick me up and take me to get something to eat and then back home for the day.
I did make what felt like a couple extra bathroom trips that afternoon and evening. They were similar to the bathroom trips of prep day. But things were back to normal on Saturday morning.
The only real consequence was I had some swelling and bruising on the hand that had the IV in it, and I covered my hand with an extra-large Band-Aid.
That was it.
I wasn’t sore anywhere else. And I’m grateful for that but also for the fact that I got a clean bill of health.
If you have any hesitations about getting a colonoscopy because of post-procedure issues, you shouldn’t. If still concerned, talk to your doctor. Or the nurse who does all the work for the doctor.
As a brief aside, as I was writing this Wednesday afternoon, I got a text message from my doctor, Doug Stokes, just following up with me.
‘Free’ screening? Know your rights to get no-cost care
KAISER HEALTH NEWS — An ounce of prevention … well, you know the rest. In medicine, prevention aims to spot problems before they worsen, affecting both a patient’s health and finances.
One of the more popular parts of the Affordable Care Act, which allows patients to get certain tests or treatments without forking out cash to cover copayments or deductibles, is based on that idea.
“There are still some gaps that need to be filled,” said Katie Keith, a researcher at the Center on Health Insurance Reforms at Georgetown University. But, she said, the law “unquestionably” made preventive care more affordable.
Since late 2010, when this provision of the ACA took effect, many patients have paid nothing when they undergo routine mammograms, get one of more than a dozen vaccines, receive birth control, or are screened for other conditions, including diabetes, colon cancer, depression, and sexually transmitted diseases.
That can translate to big savings, especially when many of these tests can cost thousands of dollars.
Yet this popular provision comes with challenges and caveats, from an ongoing court case in Texas that might overturn it, to complex and obtuse qualifiers that can limit its breadth, leaving patients with medical bills.
KHN spoke with several experts to help guide consumers through this confusing landscape.
Their No. 1 tip: Always check with your own health plan beforehand to ensure that a test, vaccine, procedure, or service you need is covered and that you qualify for the no-cost-sharing benefit. And, if you get a bill from a physician, clinic, or hospital that you think might qualify for no cost sharing, call your insurer to inquire or dispute the charge.
Here are five other things to know:
1. Your insurance matters.
The law covers most types of health insurance, such as qualified health plans under the ACA that consumers have purchased for themselves, job-based insurance, Medicare, and Medicaid. Generally not included are pre-ACA legacy health plans, which were in existence before March 2010 and have not changed since then, and most short-term or limited-benefit plans. Medicare and Medicaid’s rules on who is eligible for what tests without cost sharing may vary from those of commercial insurance, and Medicare Advantage plans in some cases may have more generous coverage than the traditional federal program.
2. Not all preventive services are covered.
The federal government currently lists 22 broad categories of coverage for adults, an additional 27 specifically for women, and 29 for children.
To get on those lists, vaccines, screening tests, drugs, and services must have been recommended by one of four groups of medical experts. One of those is the U.S. Preventive Services Task Force, a nongovernmental advisory group that weighs the benefits and potential drawbacks of screening tests when used in the general population.
For example, the task force recently recommended lowering the age for colon cancer screening to include people ages 45 through 49. That means more people won’t have to wait for their 50th birthday to skip copays or deductibles for screening. Still, younger folks might be left out a bit longer if their health plan applies to the calendar year, which many do, because those plans are not technically required to comply until January.
This area is also one in which Medicare sets its own rules that might differ from the task force’s recommendations, said Anna Howard, a specialist in care access at the American Cancer Society Cancer Action Network. Medicare covers stool tests or flexible sigmoidoscopies, which screen for colon cancer, without cost sharing starting at age 50. There is no age limit on screening colonoscopies, although they are restricted to once every 10 years for people at normal risk. Coverage for high-risk patients allows for more frequent screening.
Many of the task force recommendations are limited to very specific populations.
For instance, the task force recommended abdominal aortic aneurysm screening only for men ages 65 to 75 with a history of smoking.
Others, including women, should get tested if their physicians think they have symptoms or are at risk. Such tests then could be diagnostic, rather than preventive, triggering a copayment or deductible charge.
3. There can be limits.
Insurers have leeway on what is allowed under the rules, but they have also been warned that they can’t be parsimonious.
California, for example, recently cracked down on insurers who were limiting cost-free testing for sexually transmitted diseases to once a year, saying that wasn’t adequate under state and federal laws.
The ACA does set parameters. Federal guidance says stop-smoking programs, for example, must include coverage for medications, counseling, and up to two quit attempts per year.
With contraception, insurers must offer at least one option without copays in most categories of birth control but are not required to cover every single contraceptive product on the market without copays. For example, insurers could choose to focus on generics, rather than brand-name products. (The law also allows employers to opt out of the birth control mandate.)
4. Some tests — often the expensive ones — have special challenges that affect coverage determinations.
As the ACA went into effect, trouble spots emerged. There was a lot of drama around colonoscopies. Initially, patients found they were billed for copayments if polyps were found. But health regulators put a stop to that, saying polyp removal is considered an essential part of the screening exam. Those rules apply currently to commercial insurance and are still phasing in for Medicare.
More recently, federal guidance clarified that patients cannot be charged for colonoscopies ordered following suspicious findings on stool-based tests, such as those mailed to patients’ homes, or colon exams using CT scanners.
The rules apply to job-based and other commercial insurance with one caveat: They go into effect for policies whose plan years start in May, so some patients with calendar-year coverage may not yet be included.
At that point, it will be “a gigantic win,” said Dr. Mark Fendrick, director of the University of Michigan’s Center for Value-Based Insurance Design.
But, he noted, Medicare is not included. He and others are urging Medicare to follow suit.
Such differences in payment rules based on whether an exam is considered a diagnostic or a screening test are a problem for other types of tests, including mammograms.
This recently tripped up Laura Brewer of Grass Valley, California, when she went in for a mammogram and ultrasound in March, six months after a cyst had been noticed in a previous exam by a different radiologist. The earlier test didn’t cost her anything, so she was stunned by her bill for more than $1,677 for procedures now considered diagnostic.
“They are giving me the same service and changed it to be diagnostic instead of screening,” Brewer said.
Georgetown’s Keith pointed out a related complication: It might not be a specific development or symptom that triggers that change. “If patients have a family history and need to get tested more frequently, that is often coded as diagnostic,” she said.
5. Vaccines and medicines can be tricky, too.
Dozens of vaccines for children and adults, including those for chickenpox, measles, and tetanus, are covered without cost sharing. So are certain preventive medicines, including certain drugs for breast cancer and statins for high cholesterol. Preexposure medications to prevent HIV — along with much of the associated testing and follow-up care — are also covered without cost to HIV-negative adults at high risk.
So, what’s next?
Overall, the ACA has helped lower out-of-pocket costs for preventive care, said Keith. But, like almost everything else with the law, it has also attracted critics.
They include conservatives opposed to some of the free services, who filed the lawsuit in a Texas federal district court that, if it prevails, could overturn or restrict part of the law that provides no cost sharing for preventive care.
A ruling in that case, Kelley v. Becerra — the latest in a series of challenges to the ACA since it took effect — may come this summer and will likely be appealed.
If the ultimate decision invalidates the preventive mandate, millions of patients, including those who buy their own insurance and those who get it through their jobs, could be affected.
“Each insurer or employer would be left to decide which preventive services to cover and whether to do so with cost sharing,” said Keith. “So even those who did not lose access to preventive services themselves could have to pay out-of-pocket for all or some preventive care.”